Fillable Do Not Resuscitate Order Template for New Hampshire
The New Hampshire Do Not Resuscitate Order form is an essential document for individuals seeking to have their wishes respected regarding the use of resuscitation techniques in the event of a cardiac or respiratory arrest. It is designed to communicate a person’s decision to forgo resuscitative measures to medical personnel, ensuring that one’s preferences about end-of-life care are understood and adhered to. This form plays a critical role in healthcare planning, allowing patients, in consultation with their healthcare providers, to make informed decisions about their treatment. The process of obtaining a Do Not Resuscitate Order involves detailed discussions with healthcare providers, ensuring that individuals are fully aware of the implications of their choices. Once signed, this document has legal authority, guiding emergency medical services and other healthcare professionals in honoring the patient's wishes. This preventive measure contributes to the autonomy individuals have over their medical care, emphasizing the importance of personal choices in healthcare situations that are often complex and emotionally charged.
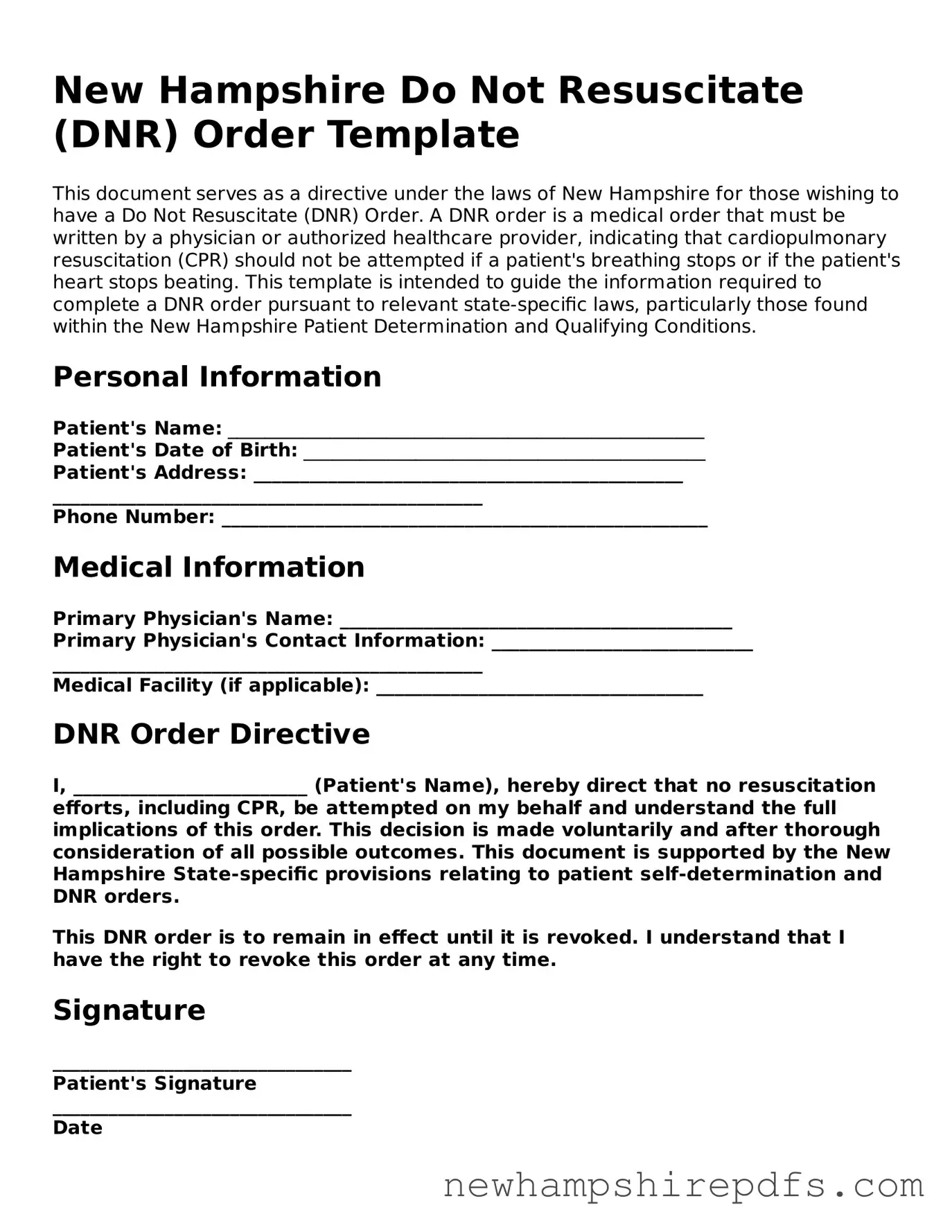
Document Sample
New Hampshire Do Not Resuscitate (DNR) Order Template
This document serves as a directive under the laws of New Hampshire for those wishing to have a Do Not Resuscitate (DNR) Order. A DNR order is a medical order that must be written by a physician or authorized healthcare provider, indicating that cardiopulmonary resuscitation (CPR) should not be attempted if a patient's breathing stops or if the patient's heart stops beating. This template is intended to guide the information required to complete a DNR order pursuant to relevant state-specific laws, particularly those found within the New Hampshire Patient Determination and Qualifying Conditions.
Personal Information
Patient's Name: ___________________________________________________
Patient's Date of Birth: ___________________________________________
Patient's Address: ______________________________________________
______________________________________________
Phone Number: ____________________________________________________
Medical Information
Primary Physician's Name: __________________________________________
Primary Physician's Contact Information: ____________________________
______________________________________________
Medical Facility (if applicable): ___________________________________
DNR Order Directive
I, _________________________ (Patient's Name), hereby direct that no resuscitation efforts, including CPR, be attempted on my behalf and understand the full implications of this order. This decision is made voluntarily and after thorough consideration of all possible outcomes. This document is supported by the New Hampshire State-specific provisions relating to patient self-determination and DNR orders.
This DNR order is to remain in effect until it is revoked. I understand that I have the right to revoke this order at any time.
Signature
________________________________
Patient's Signature
________________________________
Date
If the patient is unable to sign, a legal representative may sign on behalf of the patient:
________________________________
Representative's Name
________________________________
Representative's Relationship to Patient
________________________________
Representative's Signature
________________________________
Date
Physician's Section
The undersigned physician affirms that the above-named patient has discussed and elected a DNR order. This order is consistent with the patient's medical condition and desires.
________________________________
Physician's Name
________________________________
License Number
________________________________
Physician's Signature
________________________________
Date
Witness Section
This DNR order has been signed in the presence of the following witnesses, confirming that the patient, or their representative, has signed or acknowledged their signature on this document willingly and voluntarily.
- Witness 1 Name: __________________________________________
- Witness 2 Name: __________________________________________
Signature of Witness 1: _______________________________________
Date: ________________________________________________________
Signature of Witness 2: _______________________________________
Date: ________________________________________________________
PDF Form Breakdown
| Fact | Description |
|---|---|
| Purpose | The New Hampshire Do Not Resuscitate (DNR) Order form is used to instruct medical professionals not to perform CPR on a patient in the event of cardiac or respiratory arrest. |
| Applicable Law | The form is governed by the laws of the State of New Hampshire, under RSA 137-J: Permission to Withhold Life-Sustaining Treatment. |
| Who Can Sign | The DNR form must be signed by both the patient (if capable) or their legally recognized healthcare agent, and the patient’s attending physician. |
| Validity and Accessibility | For the order to be valid, it must be easily accessible to healthcare providers. It is often suggested to keep a copy with the patient at all times. |
How to Use New Hampshire Do Not Resuscitate Order
Filling out a Do Not Resuscitate (DNR) Order in New Hampshire requires careful attention to detail to ensure one's wishes are accurately reflected. This legal form is critical for individuals who choose not to undergo cardiopulmonary resuscitation (CPR) in the event of cardiac or respiratory arrest. The process of completing this form is straightforward but demands precision. Here's a breakdown of the steps needed to accurately fill out the New Hampshire DNR Order form.
- Begin by obtaining the most current version of the New Hampshire Do Not Resuscitate Order form. This ensures that all the information provided is up to date and in compliance with New Hampshire state laws.
- Enter the patient's full name at the top of the form, ensuring that it matches the name on their official identification documents to avoid any confusion or ambiguity.
- Provide the patient's date of birth in the format specified on the form to verify the patient's identity and age accurately.
- Document the patient's full home address, including street, city, state, and zip code, to ensure there is no confusion regarding the patient's residence or where the DNR order should be applied.
- Indicate the patient's medical condition in the section provided. This requires a clear and concise description of the patient's current health status and why a DNR order is being requested.
- A licensed physician must review the details provided, sign the form, and include their medical license number. This step is crucial as it validates the DNR order.
- The patient or their legally authorized representative (if the patient is unable to sign) must sign and date the form. If a representative is signing, their relationship to the patient must be clearly indicated.
- Finally, ensure that all necessary contact information for both the patient and the physician is included on the form. This includes phone numbers and addresses.
- Review the entire document to ensure that all information is correct and that no sections have been missed.
- Keep the completed DNR Order form in an easily accessible location and inform family members or guardians of its existence and location. It’s also advisable to keep a copy with your personal medical records.
After completing the New Hampshire Do Not Resuscitate Order form, the next steps involve ensuring that the form is easily accessible in the event of an emergency. A copy should be given to the patient's primary care physician to be included in their medical records, and it may also be beneficial to inform close family members or caregivers about the existence and importance of this document. In New Hampshire, having a DNR Order in place is critical for those who wish to avoid CPR or advanced life support interventions, making this document an essential part of health care planning for individuals facing end-of-life decisions.
Understanding New Hampshire Do Not Resuscitate Order
What is a Do Not Resuscitate (DNR) Order in New Hampshire?
A Do Not Resuscitate (DNR) Order in New Hampshire is a medical order that is written by a doctor. It instructs health care providers not to do cardiopulmonary resuscitation (CPR) if a person's heart stops or if they stop breathing. This order is used for people who are near the end of their life or have a terminal illness and want to die naturally, without aggressive interventions.
How can someone get a DNR Order in New Hampshire?
The process starts with a conversation between a patient and their doctor. If a DNR is considered to be in the best interest of the patient, the doctor can fill out and sign the DNR Order form. It’s important for the patient to discuss their wishes with family members or caregivers so that they understand the patient's preferences. The form should then be kept in a place where it is easily accessible to emergency personnel.
Is a DNR Order permanent, or can it be changed?
A DNR Order is not permanent and can be changed or revoked at any time by the patient. If a patient changes their mind, they should discuss their new wishes with their doctor. A new form may need to be completed to reflect these changes. Additionally, it's recommended to inform family members of any changes to ensure they understand the current wishes regarding resuscitation efforts.
What should someone do with their DNR Order once it's completed?
Once a DNR Order is completed, it should be placed in an easily accessible location. Many people choose to keep it on their refrigerator or in their wallet. A copy of the DNR Order should also be given to the patient's primary care doctor and any specialists they may have. It's crucial to inform family members and caregivers about the location of the DNR Order so they can provide it to emergency personnel if necessary.
Common mistakes
Filling out the New Hampshire Do Not Resuscitate (DNR) Order form is an important step for those who wish to specify their preferences regarding emergency medical interventions. However, mistakes in completing this form can lead to confusion and unwanted medical treatments. Here are five common errors:
- Not consulting a healthcare provider: A DNR form requires the input and signature of a qualified healthcare provider. A common mistake is attempting to complete the form without consulting a healthcare professional. This oversight can invalidate the form, as the healthcare provider's assessment and agreement are crucial to its legitimacy and enforcement.
- Using incorrect or incomplete patient information: Every detail on the DNR form needs to be accurate. Incorrect patient information, such as misspelled names or wrong dates of birth, can lead to confusion in emergency situations. It is essential to double-check all personal information for accuracy.
- Failing to communicate wishes with family and healthcare proxies: Even with a valid DNR order, if family members or healthcare proxies are unaware of the individual's wishes, disputes or delays in care might occur. Ensuring that close family members and any appointed healthcare proxies are informed and understand the DNR order is critical for its effective implementation.
- Not keeping the DNR form accessible: In an emergency, healthcare providers need immediate access to the DNR order. A mistake many make is filling out the form but keeping it in a place where it is not easily found. It's recommended to keep the form in a visible and accessible location and to inform family members and healthcare providers of its location.
- Forgetting to review and update: A DNR order reflects a person's wishes at a specific point in time. However, preferences and medical conditions can change. Not regularly reviewing and updating the DNR order can lead to a disconnect between the current wishes of the individual and the instructions in the DNR order. It is advisable to review the DNR order periodically, especially after any significant change in health status.
To avoid these mistakes, it's important to take the process seriously and ensure all procedures are correctly followed. Engaging in open communication with healthcare providers, family members, and healthcare proxies, as well as keeping the document up-to-date and accessible, are key steps in ensuring that your wishes are respected and followed.
Documents used along the form
When preparing for medical care planning, especially in cases where life-sustaining treatments are declined, such as with a Do Not Resuscitate (DNR) Order, several important documents should be considered alongside it. These not only support the individual’s wishes but also guide family members and healthcare providers through the necessary steps during critical times. Below is a list of documents often used in conjunction with a New Hampshire DNR Order.
- Advanced Directive: A legal document that outlines a person’s wishes regarding medical treatment, should they become unable to communicate those wishes directly.
- Medical Power of Attorney (POA): Designates a person (agent) to make healthcare decisions on behalf of the individual if they are incapacitated.
- Living Will: Specifies the types of medical treatments and life-sustaining measures an individual wants or does not want, such as mechanical ventilation or tube feeding, at the end of life.
- Physician Orders for Life-Sustaining Treatment (POLST): A medical order that details the specific types of life-sustaining treatment an individual wishes to receive or avoid, based on their current health condition.
- Healthcare Proxy: Assigns a healthcare agent to make medical decisions on behalf of the individual, similar to a Medical Power of Attorney, but may include more specific instructions or limitations.
- Emergency Contact Information: Lists contacts for emergency situations, including family members, friends, and healthcare agents, along with phone numbers and addresses.
- HIPAA Release Form: Authorizes the disclosure of an individual’s protected health information to designated persons.
- Organ and Tissue Donation Registration: Expresses an individual’s intent to donate their organs and tissues for transplantation after death.
- Last Will and Testament: Outlines how an individual’s property and assets are to be distributed after their death. While not directly related to medical decisions, it is often part of end-of-life planning.
These documents serve as critical components of a comprehensive healthcare planning strategy, ensuring that an individual’s preferences are respected and legally recognized. Each plays a distinct role in communicating wishes to family members and medical professionals, thereby reducing the burden of decision-making in difficult times. Familiarizing oneself with these documents and discussing them with loved ones and healthcare providers can significantly impact the effectiveness of a DNR Order and other advanced healthcare directives.
Similar forms
The New Hampshire Do Not Resuscitate Order form is similar to several other legally significant documents used within the healthcare field. These documents are primarily utilized to make a patient's wishes known in advance, particularly in situations where the patient may not be able to communicate these wishes directly to healthcare providers. The comparison to these documents sheds light on the broader context of patient rights and the scope of medical directives.
The form closely mirrors the Advance Healthcare Directive, often simply referred to as a living will. Like the Do Not Resuscitate Order, an Advance Healthcare Directive allows individuals to outline specific medical treatments they do or do not wish to receive in the event they are incapacitated and cannot make decisions for themselves. Both documents serve as a means for individuals to express their healthcare preferences, but while the Do Not Resuscitate Order specifically addresses the issue of resuscitation, the Advance Healthcare Directive covers a broader range of medical interventions and treatments.
Similarly, the form is akin to the Medical Orders for Life-Sustaining Treatment (MOLST). This document also specifies a patient's preferences regarding the use of life-sustaining measures, including intubation, mechanical ventilation, and other forms of medical intervention aimed at prolonging life. The main distinction lies in the scope and detail provided by MOLST, which, like the Do Not Resuscitate Order, is designed for use by patients with serious health conditions. Both documents are instrumental in guiding healthcare professionals in emergency or critical care situations to align their interventions with the patient's wishes.
The Power of Attorney for Health Care (POA-HC) is another document with similarities to the New Hampshire Do Not Resuscitate Order. The POA-HC designates a surrogate to make healthcare decisions on behalf of the patient if they are unable to do so themselves. While the essence of the POA-HC is to appoint a decision-maker rather than to specify particular medical treatments, it complements the Do Not Resuscitate Order by ensuring that the patient's overall healthcare directives, including the wish not to be resuscitated, are honored by someone who understands the patient's values and desires.
Dos and Don'ts
When dealing with the New Hampshire Do Not Resuscitate (DNR) Order form, individuals face a sensitive and crucial task. The following list includes essential dos and don'ts to guide you through this critical process.
- Do read the instructions carefully before you start filling out the form to ensure that you understand every aspect of the DNR order.
- Do confirm the patient’s eligibility for a DNR order with a healthcare provider to ensure it aligns with their current health condition and wishes.
- Do use black ink for clarity and legibility, which is vital for the readability of the document in emergent situations.
- Do ensure that all information provided on the form is accurate and matches the patient's official identification documents to avoid any confusion or discrepancies.
- Do have the form signed by the authorized healthcare provider as their signature is crucial for the legality of the DNR order.
- Don't leave any sections blank. If a section does not apply, fill it with "N/A" (not applicable) to indicate that it was not overlooked.
- Don't attempt to alter the form after it has been completed and signed, as this may void its validity.
- Don't forget to make sufficient copies. Keep one with the patient and distribute others to relevant family members and healthcare providers.
- Don't hesitate to ask for help from a healthcare provider or legal professional if you have any questions about the DNR order or the completion of the form.
Misconceptions
Regarding the New Hampshire Do Not Resuscitate (DNR) Order form, several misconceptions contribute to misunderstandings. Clarifying these misconceptions ensures individuals are better informed about their healthcare choices and the implications of such orders.
Misconception 1: A Do Not Resuscitate Order form applies to all medical treatments. This is incorrect; the form specifically pertains to not initiating cardiopulmonary resuscitation (CPR) in the event of a patient's cardiac or respiratory arrest. It does not preclude the patient from receiving other forms of medical care.
Misconception 2: The form is permanent and irrevocable. Patients possess the right to revoke their DNR order at any time. They can communicate their wish to revert the decision either verbally or in writing, contingent upon their capacity to make healthcare decisions.
Misconception 3: Only the elderly or terminally ill can request a DNR order. Any individual, regardless of age or health status, may discuss and opt for a DNR order with their healthcare provider, providing they fully understand the implications of such a decision.
Misconception 4: The form negates the need for an advance directive. While a DNR order is a directive pertaining to the specific instance of cardiopulmonary resuscitation, an advance directive is a broader document that covers a wide range of end-of-life care decisions. It's advisable for individuals to have both if they wish to comprehensively dictate their care preferences.
Misconception 5: A verbal request by a patient for a DNR is sufficient. In New Hampshire, formal documentation is required to validate a DNR order. Although emergency responders respect expressed wishes to the extent possible, legally recognized documentation ensures clarity and adherence to the patient's wishes.
Misconception 6: The DNR form is only effective in hospital settings. The DNR order is recognized across various settings, including but not limited to hospitals, nursing homes, and private residences. The scope of acknowledgment ensures the patient's wishes are honored in diverse environments.
Misconception 7: Only physicians can authorize a DNR order. While a physician's signature is indeed required, the initiation of the process often comes from the patient or the patient's health care proxy or guardian, demonstrating shared decision-making in the patient's healthcare.
Misconception 8: The DNR order impacts the quality of care provided. Healthcare professionals are committed to offering the highest standard of care to all patients. The existence of a DNR order does not affect the quality or the range of other medical treatments provided to the patient.
Understanding the facts behind these misconceptions is crucial for individuals contemplating their healthcare preferences and end-of-life decisions. It ensures decisions are based on accurate information and that the care received aligns with their wishes.
Key takeaways
When considering a Do Not Resuscitate Order (DNR) in New Hampshire, understanding the key elements of the form and its implications is crucial. This process ensures that the wishes of individuals regarding resuscitation in the event of a cardiac or respiratory arrest are respected and followed. Here are the essential takeaways about filling out and using the New Hampshire Do Not Resuscitate Order form:
- Understanding the purpose: The DNR order is specifically designed to prevent emergency medical personnel from performing CPR (cardiopulmonary resuscitation) in case your heart stops or you stop breathing. This is an important decision that should be considered carefully.
- Discuss with healthcare provider: It's vital to have a thorough discussion with your healthcare provider about your health condition, prognosis, and the implications of a DNR order. This decision should be informed and voluntary.
- Valid form requirement: The DNR order must be completed on a valid form that is recognized by the state of New Hampshire. Make sure you are using the correct document to avoid any future complications.
- Signature necessary: The form requires signatures from both the patient (or legal healthcare decision-maker, if the patient is unable) and the healthcare provider to be valid. This signifies that there has been an agreement between both parties regarding the DNR status.
- Availability of the form: Once completed, the DNR form should be kept in a place where it can be easily found by emergency personnel. This could mean placing it on the refrigerator, by your bed, or in another prominent location if you're at home.
- Inform family and caregivers: It's important to communicate your decision to have a DNR order with family members and caregivers. This ensures that they understand your wishes and can help advocate for those wishes in case of an emergency.
- Wearing DNR identification: In some cases, patients may choose to wear DNR bracelets or necklaces as a form of identification to alert emergency personnel of their DNR status. This can be especially useful if the patient is not at home.
- Revocation is possible: The decision to have a DNR order is not final and can be revoked at any time by the patient or their legal healthcare decision-maker. This should be communicated immediately to the healthcare provider to update the medical records.
- Legal protection: Emergency medical technicians and other healthcare providers are legally protected when they follow a valid DNR order. This means they cannot be held legally responsible for adhering to the wishes outlined in the form.
Taking these key points into consideration can help ensure that the process of filling out and utilizing a Do Not Resuscitate Order in New Hampshire goes smoothly, respecting the wishes of individuals at a critical time. Always remember, this is a personal and significant decision that should be made with careful thought and consideration.
Some Other New Hampshire Forms
New Hampshire Power of Attorney - It’s recommended to keep a copy of this document accessible and inform key people of its location and contents.
Nh Divorce Laws Adultery - Provides a level of protection for both parties by detailing the separation terms in a legally recognized format.